Why are ethnic minorities more vulnerable to coronavirus?
Experts say health issues, socioeconomic inequality and discrimination among factors, as UK government announces review.

London, United Kingdom – In late February, Amged el-Hawrani, a 55-year-old ear, throat and nose consultant, was showing mild signs of coronavirus, but put feelings of exhaustion down to his gruelling shifts at the University Hospitals of Derby and Burton.
Despite having no underlying health issues, his condition deteriorated.
Keep reading
list of 4 itemsMexico’s teachers seek relief from pandemic-era spike in school robberies
‘A bad chapter’: Tracing the origins of Ecuador’s rise in gang violence
Why is the US economy so resilient?
On March 4, he was admitted to Glenfield Hospital in Leicester. Three weeks later, on March 28, he died of COVID-19.
He was among the first 10 British doctors to die from the disease, all of whom were all from Black and minority ethnic (BME) backgrounds.
“It may be a coincidence,” el-Hawrani’s brother, Amal, told Al Jazeera. “It may be a genetic element where certain people from a particular region in the world are predisposed to succumbing to the virus.”
According to a tally by Al Jazeera, some 70 percent of at least 50 healthcare workers who have so far died of coronavirus in the UK have ancestry in other regions including Asia, Africa and the Middle East, alarming statistics that prompted calls to investigate why this is happening.
You've got a high proportion of BAME people not able to stay at home, serving the nation, putting themselves at risk.
On Thursday, the government heeded those calls, which were led by Chair of the British Medical Association Chaand Nagpaul, and promised a formal review into why BME communities appear to be more vulnerable.
Amal was among those who welcomed the move; the review is expected to begin in the coming days.
About 20 percent of the UK belongs to an ethnic minority, according to a 2011 census.
Forty percent of NHS staff are from BME backgrounds, a number which rises to 45 percent in London, an epicentre of the pandemic.
The capital is home to the UK’s highest ethnic minority population, 40.2 percent.
As well as healthcare workers, BME communities among the wider population are disproportionately affected by the coronavirus.
Data published on April 11 by the Intensive Care National Audit and Research Centre (ICNARC) found that one-third of over 2,000 critically ill coronavirus patients were from BME backgrounds.
![Composite - Dr Adil El Tayar (L), Dr Amged (C), Dr Habib Zaidi Credit (R) [NHS]](/wp-content/uploads/2020/04/5a66b55a426a4cbf91720508de4d71f1_18.jpeg)
Azeem Majeed, a professor of primary care at Imperial College in London, said that while the reason ethnic minorities were more vulnerable was unclear, comorbidities – the presence of more than one disease or condition in a patient at the same time – might be among the factors.
“It could be related to underlying medical problems such as diabetes and kidney disease,” Majeed told Al Jazeera.
There are also concerns that social and economic inequality, which impacts minority communities more starkly, could be playing a role.
“You’ve got a high proportion of BAME people not able to stay at home, serving the nation, putting themselves at risk,” said the BMA’s Nagpaul. “And if you add that to overcrowded and multigenerational occupancies, the infections can be brought back home and spread to other members of the family.”
Overcrowding affects 30 percent of Bangladeshi and 15 percent of Black African households in the UK, compared with about 2 percent of white households in the UK, government data suggests.
Zubaida Haque, the deputy director of race equality think-tank Runnymede Trust, said it was important to note that BME NHS staff were likely more privileged and therefore able to afford better living conditions.
“On average, doctors will be different from your average Black and minority person in the community, in terms of housing conditions and the area they live in, because socioeconomically they’re better off,” she said.
“We know that if you’re from a more disadvantaged background, you have worse health outcomes.”
Haque warned, however, that structural racial inequalities impacted non-white people, regardless of their class status.
“We know that BME NHS staff can’t complain as much because they’re worried about the recriminations of complaining,” she said.
“They’re much likely to be harassed and face discrimination compared to their white counterparts. There is the question of, did they have the appropriate PPE equipment? If they didn’t, did they feel they could complain or were they worried about the recriminations from complaining?”
According to a poll on Thursday, 75 percent of healthcare workers in the UK believe the government has failed to protect them amid the coronavirus pandemic.
Nagpaul also pointed to institutional racism in the medical profession, saying it loaded pressure on ethnic minority NHS staff.
“BME doctors often feel bullied and harassed at higher levels compared to their white counterparts,” he said, “and they are twice as likely not to raise concerns because of fears of recrimination.”
A report commissioned last year by the General Medical Council (GMC), the regulatory body for doctors in the UK, found employers and healthcare providers were more likely to refer doctors from BME backgrounds who obtained their primary medical qualification outside the UK to the GMC, compared with their white or UK qualified peers.
Earlier this year, the BMA warned that British ethnic minority medical students experience racial harassment on campus and during work experience.
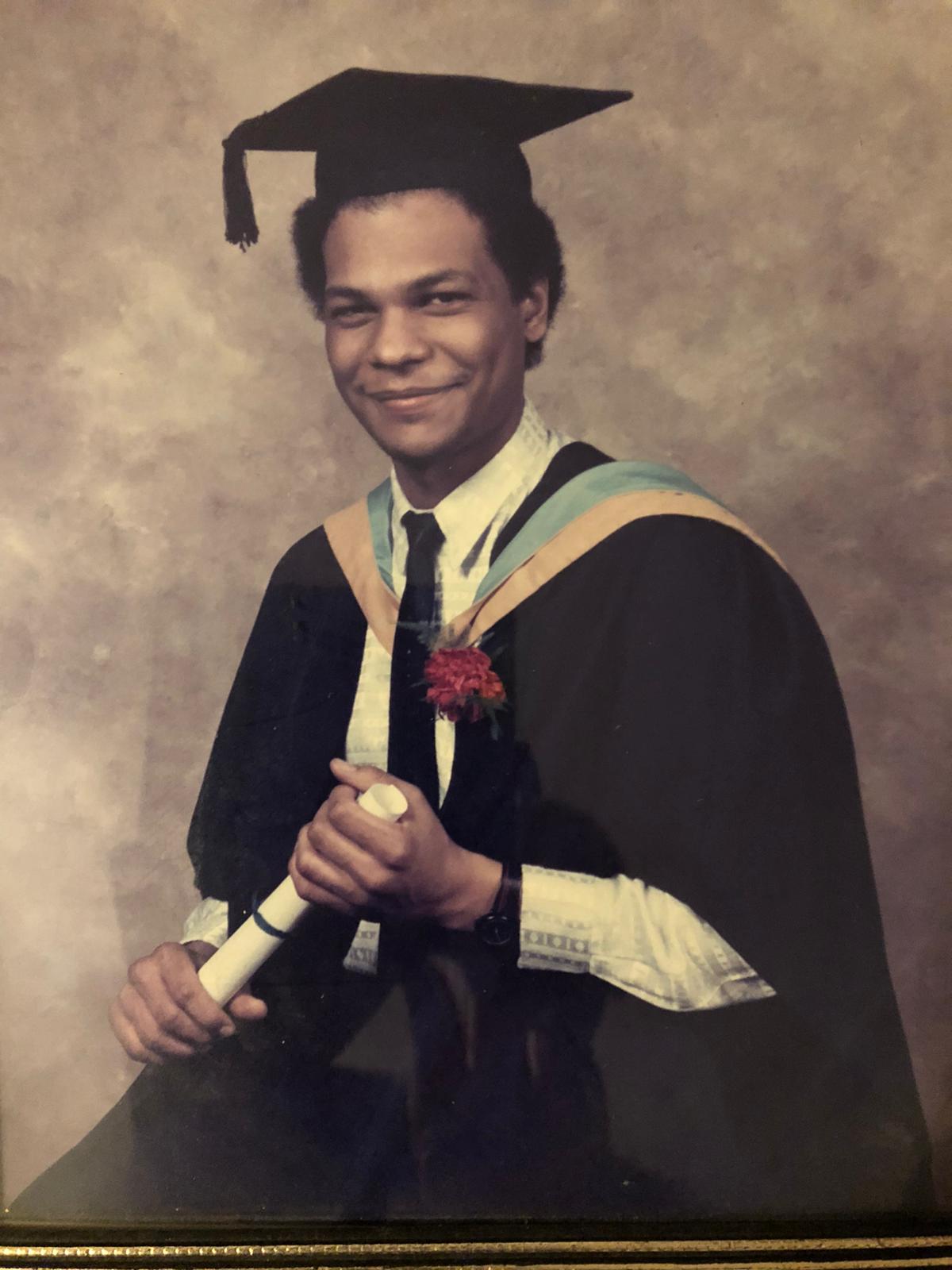
For Amal, the disproportionate number of deaths highlighted the “prejudice in the system”, and reminded him of his late brother’s student days.
“When Amged graduated and he was training as a doctor, he was sent far away from any of his desired locations. I remember him saying to me, ‘All I see my front window is sheep, and all I see from my back window are cows.’ Whereas some of his British white counterparts would get London, Manchester, Birmingham, Liverpool – the major cities.”