US panel advises breast cancer screenings should begin at age 40
Lowering age for biennial screenings could result in more lives being saved, US health task force says.
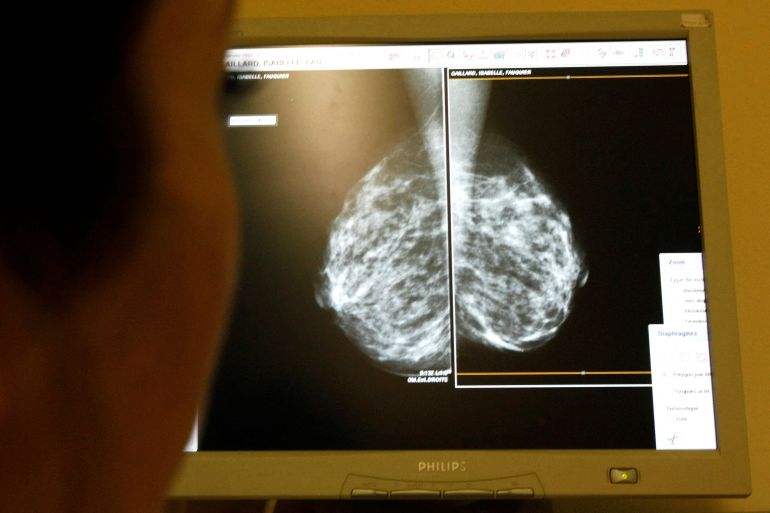
Women should begin getting mammogram screenings for breast cancer at age 40, an influential United States health panel has advised, in a move the US Preventive Services Task Force (USPSTF) said could help save thousands of lives.
The panel’s update on Tuesday reverses a controversial recommendation made in 2009, when it said biennial screening should start a decade later – at age 50 – unless women and their doctors decided earlier checks were appropriate.
Keep reading
list of 3 itemsBreast cancer: A complete guide
Is ‘Pinktober’ helping or hurting breast cancer awareness?
The task force, a group of independent experts appointed by the US Department of Health and Human Services, said that while it previously recommended women in their 40s make individual choices about when to start screening, the new guidance could result in 19 percent more lives being saved.
“This new recommendation will help save lives and prevent more women from dying due to breast cancer,” Dr Carol Mangione, the immediate past chair of the USPSTF, said in a statement (PDF).
Breast cancer is the second-most common cancer and the second-most common cause of cancer death for women in the United States, killing approximately 42,000 women and 500 men, according to official data. Black women are 40 percent more likely to die than white women.
The guidance is still considered a draft, with the Task Force posting the evidence it considered on its website and allowing public comments and review until early June. US health insurance is required to cover any service the USPSTF recommends, regardless of cost.
“Ensuring Black women start screening at age 40 is an important first step, yet it is not enough to improve the health inequities we face related to breast cancer,” the task force’s vice chair, Wanda Nicholson, said.
“In our draft recommendation, we underscore the importance of equitable follow-up after screening and timely and effective treatment of breast cancer and are urgently calling for more research on how to improve the health of Black women.”
The draft recommendation applies to women at “average risk” of breast cancer, which includes people with a family history of breast cancer or other risk factors such as having dense breasts, which about half of all women do.
It does not apply to people who have a prior history of breast cancer, or who have certain genetic markers that place them at high risk, have had high-dose radiation therapy from a young age, or had high-risk lesions taken on biopsies.
The American Cancer Society (ACS) applauded the updated USPSTF recommendation to begin screening at age 40.
However, the group’s chief scientific officer, Dr William Dahut, said in a statement that the ACS recommends annual mammograms because “current evidence indicates that biennial screening in [women under age 55] is associated with a diagnosis of more advanced disease”.
The spokesperson for the American College of Obstetricians and Gynecologists, Dr Christopher M Zahn, said in a statement that the group “has long asserted that regular screening via mammography starting at 40 years reduces breast cancer mortality in those without additional risk factors”.
“Recognizing that Black women are more likely to die of breast cancer than white women, [the earlier start to screening] could help make a meaningful difference in ensuring that more Black women are diagnosed earlier,” Zahn added.