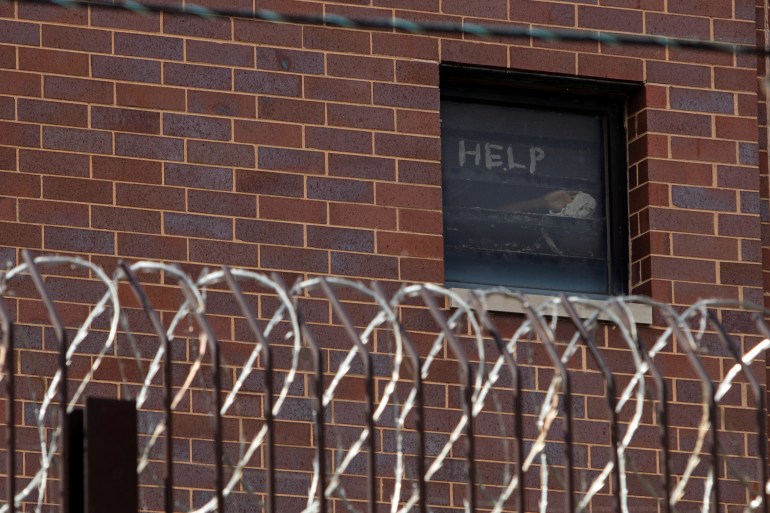
‘A living hell’: Inside US prisons during the COVID-19 pandemic
Prisoners and their families describe the emotional, physical and financial toll of the pandemic.

In the days before Christmas, 44-year-old April Harris sat in her prison cell at the California Institution for Women for more than 23 hours a day. In the 20 minutes she was allowed to leave it, she and the other prisoners would flood into the common areas – choosing either to take a shower or to make a short phone call.
Restrictions have fluctuated during the various lockdowns implemented throughout the COVID-19 pandemic, but in the 11 months since the California Department of Corrections and Rehabilitation (CDCR) first banned visitations across state prisons, Harris says she has seen the mental health of those around her steadily deteriorate.
Keep reading
list of 4 itemsMexico’s teachers seek relief from pandemic-era spike in school robberies
‘A bad chapter’: Tracing the origins of Ecuador’s rise in gang violence
Why is the US economy so resilient?
“A friend of mine sliced her arms yesterday because she said that she couldn’t handle it anymore,” Harris wrote at the end of 2020 in a message sent via JPay, an electronic messaging system used in prisons.
“Women scream, beat their doors and call fake medical emergencies just to get out of their rooms. The women are definitely breaking.”
Elizabeth Lozano, 46, used to work in the gym, visit the law library and take art therapy and creative writing courses at the Central California Women’s Facility (CCWF) where she is imprisoned, but that all stopped in mid-March. At first, she says she was still allowed outside at intervals – first every other day and then every four days. Now, however, she says she has not smelled fresh air since late December, when the CCWF further restricted movements as the number of COVID cases rose.
“The stress level is super high,” Lozano wrote through JPay, noting that the anxiety was driven by fear of COVID in rooms where women were “packed like sardines.
“We have no control of what [others] do, so even if I take precautions [it] doesn’t mean a roommate is. We can’t social distance or shelter in place safely.”
Lawyer Penny Godbold represents individuals with disabilities in California prisons and says, “The pandemic has had an unbelievable toll on the mental health of people incarcerated in California. People describe watching others – friends, cellmates, those in their housing units – get sick and die around them without knowing whether they, too, will suffer the same fate.”
Six feet apart
Kassan Messiah, 55, last saw Lorraine, his wife of 27 years, in October, when she visited New York’s Sing Sing Correctional Facility. The visit buoyed Kassan.
“My wife is my respirator; my understanding of the world beyond the wall is all attributed to wifey,” Kassan wrote in a message sent over JPay.
But, “after each visit”, Kassan says he experiences “deflation”.
They had not seen each other since January 2020, when their communication and visits were upended.
At the beginning of January 2021, Lorraine only received one call from Kassan a week. Afraid of missing it, she kept her phone with her at all times. But sometimes, just five minutes into the call, she says she would hear the guards yelling at him to hang up.
Then, on January 23, Kassan says he was left with a bloodied mouth, a black eye, bruising and wrist lacerations after he was attacked by guards. When asked about this, the New York Department of Corrections and Community Supervision said they were investigating the incident and would not comment further. Kassan was moved into a Special Housing Unit, where he is able to call Lorraine every day. She says she now gets to hear her husband’s voice more than at any other point during the pandemic.
During her October visit to Sing Sing, social distancing restrictions prevented them from hugging. About two dozen cafeteria tables filled the visiting room. The length of the table, about six or seven feet, separated Kassan from Lorraine.
“It’s more torture than anything else because you’re so close, but yet you’re so far,” Lorraine reflected. “If you’re allowing me into the facility, why am I not able to touch his hand?”
Even so, she had gotten closer than most people with imprisoned family members.
‘Absolutely no support’
In March, as the World Health Organization (WHO) declared a pandemic, US prisons shut down visitations. A handful of states, including New York, restored visits but stopped them again months later. As of early February, only six states and the Federal Bureau of Prisons currently allow personal visits, with varying restrictions. North Carolina only allows one 30-minute visit per month; only two people can visit each time, and no children under 12 are allowed. New Hampshire allows one 45-minute each month. Visits are non-contact and nobody under 18 is allowed into facilities.
Imprisoned people “can’t see friends, and they can’t maintain consistent contact with supports, but they also can’t go to mental health programming,” said Stefen Short, the Supervising Attorney of the Prisoners’ Rights Project run by the New York-based Legal Aid Society. “Well then what’s available to this person? At the middle of a global pandemic, when everybody’s at heightened anxiety, our clients are getting absolutely no support.”
Access to legal representation has also been affected by visitation changes. Earlier this month, 31 prison systems permitted legal visitations but banned personal visits, while 13 forbade all guests. Jails have quarantined new arrivals for 10 to 14 days and only allowed detainees to place calls to lawyers for 15 to 30 minutes each day, according to Corene Kendrick, the deputy director of the ACLU’s National Prison Project.
“It’s critical for defence attorneys to meet with their clients soon after they are arrested so that the attorney can get a thorough account from their clients about witnesses, locations, possible alibi evidence, and to review documents, police reports, and photos, and explain the next steps in the process to the client. Regardless of whether it is in the intake quarantine areas or in the general population sections, most jails often have very few or no options to set up confidential video or telephone calls,” Kendrick explains.
“In prisons, where people may need to speak to their attorney for purposes of a pending appeal, a new lawsuit, or as part of a class-action lawsuit regarding conditions, there are the same limitations.”
‘An ongoing nightmare’
For those with pre-existing mental health conditions who are no longer able to see their therapists, the strain has been even greater.
“It’s a living hell, pretty much,” says one California prisoner, who has been diagnosed with borderline personality disorder and went seven months last year without seeing his social worker. “I can only describe it as an ongoing nightmare.”
Incarceration facilities have, for decades, teemed with people needing mental healthcare. Forty-four states have an incarceration facility detaining more mentally ill people than the state’s largest psychiatric hospital, according to the Treatment Advocacy Center. Thirty-seven percent of people in state and federal prisons and 44 percent of those in jails have been diagnosed with a mental illness. Yet only 37 percent of people held in prisons and 38 percent of people detained in jails with mental health disorders were actually receiving treatment, according to a 2017 Department of Justice report.
But, during the pandemic, while the need for mental healthcare has peaked, the limited services offered in prison have diminished further.
“We’re not seeing counselors or [therapists] right now at all,” Lozano wrote via JPay. Group therapy sessions, which she attends to help with depression, have been shut down since spring, and she sees her therapist much less frequently than before the pandemic. “At one point I was quarantined in isolation and I kept asking to see mental health for that day following protocol, but I wasn’t able to see no one for days.”
“The well-being and safety of the incarcerated population and staff within CDCR and CCHCS [California Correctional Health Care Services] is our top priority,” CDCR Press Secretary Dana Simas wrote in an email statement to Al Jazeera, noting that prisoners are provided with ongoing mental health assessments and the department is conducting crisis intervention to prevent suicides.
“An incarcerated person may request mental health services or they may be referred through institution staff. Mental health and operations leadership meet daily to ensure mental health referrals and requests for services from patients are quickly addressed.”
But imprisoned people and their advocates say that even if services are formally offered, obtaining useful care is often difficult.

After a transgender man in the California Institution for Women – the facility housing April Harris – attempted suicide in May, the prison offered colouring books and crossword puzzles to prisoners. In June, a Virginia prison distributed a “mental minute” newsletter offering tips for relaxation and sleeping. The pamphlet instructed readers to “prepare yourself before going to bed” by exercising earlier in the day, “taking time to relax by meditating, listening to restful music, completing relaxation exercises or reading”.
In September, the Southern Center for Human Rights, an organisation that represents people in the criminal justice system, urged the Department of Justice to investigate “deplorable conditions” in Georgia prisons, after suicides reached unprecedented levels. In the eight months before the letter was sent, 19 people in Georgia prisons died by suicide – a rate twice the national average for suicides in state prisons. About 30 percent of the suicides occurred in a facility that “purportedly specialises in the housing and care of people with serious mental illness,” the letter said.
Employees in a Louisiana prison began walking around once a week, shouting “mental health”. One man, who asked to remain anonymous for fear of retaliation, scoffed at the idea that anyone would try to take advantage of these services. “You don’t show no signs of weakness because there’s a predatory aspect in the environment. You don’t want to be labelled or exposed or even perceived as needing that kind of help. Not to mention the level of stigma that comes with it.”
Even if someone did request help, he doubted he would receive assistance. Instead, he said, men were walking around, having full conversations with themselves.
“If you’re not bleeding, and it’s not obvious that you’re in dire need of medical [help], you’re probably going to be charged with malingering.”
‘They had no record of me’
For many of those who get COVID-19, the situation rapidly deteriorates.
Less than a month before the pandemic tore through New York City, the United Nations special rapporteur on torture rebuked the “excessive use” of solitary confinement in US correctional facilities.
“This deliberate infliction of severe mental pain or suffering may well amount to psychological torture,” Nils Melzer, the rapporteur, said.
Throughout the pandemic, the use of solitary confinement has skyrocketed, as prisons seek to stop the virus from spreading.
While overcrowding has propelled the spread of COVID-19 through prisons, it also leaves facilities with few places to quarantine infected people. In June, a coalition focused on ending solitary confinement released a report estimating a 500 percent increase in the number of people held in isolation – a violation of CDC guidelines saying “staff should ensure that the conditions in medical isolation spaces are distinct from those in punitive isolation”.
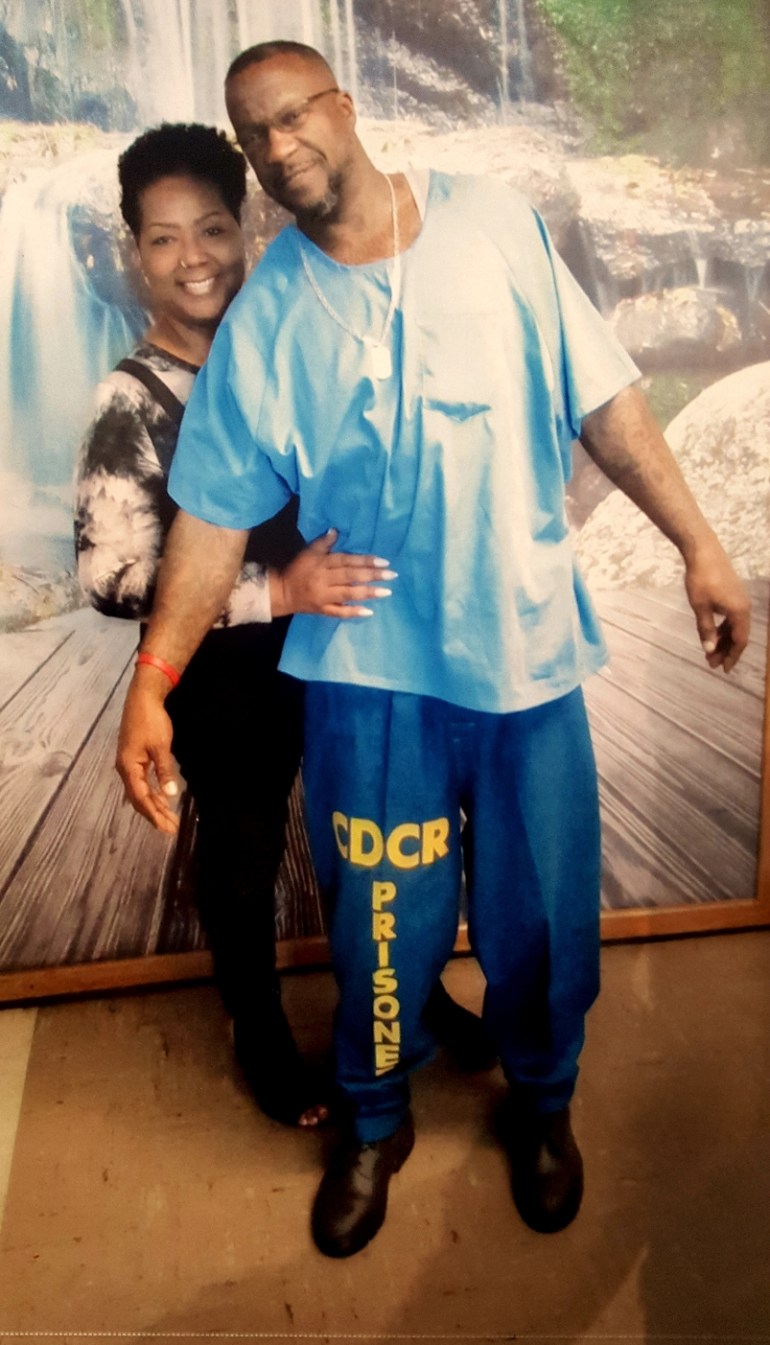
As COVID raged through California’s San Quentin State Prison, Patricia Zinnamon’s husband, Rashiyd, who had tested positive, was placed in solitary confinement, without access to a phone. He was told in June that he would be in solitary for two weeks. Rashiyd was not released until August.
Another person imprisoned at San Quentin, who asked to remain anonymous because he was communicating with a contraband mobile phone, was taken into solitary. He was told he would spend 10 to 12 days in isolation but was kept there for two months.
“The first two weeks I was in the hole, no one from medical checked on me or even knew I was there,” he says. “After the first two weeks, I stopped a nurse walking by to ask when I would be returned to my regular cell. That’s when she asked who I was and said they had no record of me.”
In the chaos, he says, correctional officers simply forgot about him.
Lawyers and academic experts say that as COVID has spread, prisons have restricted the amount of information they release, including about the number of deaths and the use of solitary confinement.
Researchers “don’t have a good understanding of exactly how states are utilising solitary confinement,” explains Lauren Brinkley-Rubinstein, a professor at the University of North Carolina School of Medicine. “The collateral consequences of COVID are really severe, and we also don’t yet know how bad it actually is.”
Research has indicated that solitary confinement causes lasting damage. In the first year after their release, people placed in solitary confinement are 78 percent more likely to die from suicide than those who were not. Those kept in restrictive housing for any period were also 127 percent more likely to die of an opioid overdose in the first two weeks post-release. A recent report focused on New York state prisons found that the suicide rate in solitary confinement was more than five times greater than that of the general prison population.
For some of those already in solitary confinement, the conditions have deteriorated even further.
Kwame Shakur, 30, who has been in solitary confinement at Indiana’s Wabash Valley Correctional Facility for more than four years, and in the facility’s long-term segregation area for nearly two and a half years, says he was not allowed outside for a month and a half in late autumn and early winter.
Shakur says guards used to walk him, hands cuffed behind his back and attached to a dog leash, to a small recreation area once a day. Shortly before Thanksgiving, the prison went into a complete lockdown. Shakur lost his daily hour in the recreation yard, which he describes as being the size of a dog kennel, until early January.
Although Shakur lost his access to the recreation area while the prison locked down, he says correctional officers [COs] still interact with both COVID positive and COVID negative populations.
“The same three guards who bring us our food and take us to showers every day are the same COs that are dealing with these corona patients,” he says.
“IDOC [Indiana Department of Correction] follows the guidance of the CDC and ISDH [Indiana State Department of Health] in our facilities to address the risk of spreading COVID-19,” IDOC Chief Communications Officer Annie Goeller said in an email statement. “This has included, but not been limited to, staff screenings upon entry to the facility, dedicating staff to specific units whenever possible, requiring the use of PPE including masks by all staff, frequent sanitation within the facility and quarantining any staff who have had prolonged contact with someone who has tested positive for COVID-19.”
‘About to blow up’
The day after Christmas, family members of people being held in Richard J Donovan Correctional Facility gathered outside the Southern California institution to protest against the facility’s handling of COVID-19. Just over a dozen people, the majority of them women, attended the rally. One woman held a sign reading “Free my husband,” another poster said “COVID is a life sentence”.
Halfway through December, cases had exploded at the facility, with more than 700 people infected in a matter of weeks.

The rapid spread of COVID at Richard J Donovan had been modelled at prisons around the country for most of the year. Even as family visitations are stopped, guards and transfers of prisoners between facilities bring COVID; once inside overcrowded prisons where social distancing is impossible, the virus runs rampant. One-fifth of the people held in federal and state prisons had tested positive for COVID-19 as of December, and inconsistent testing means the number of prisoners who have contracted the virus is likely to be even higher. At least 2,419 prisoners have died.
The situation at Richard J Donovan had been predicted. In the spring, lawyers and staff voiced concern about inadequate safety precautions and overcrowding. Advocates urged the state to release prisoners. Then, as cases began climbing across the system in late autumn, Stephanie Johnson got a concerning call from her best friend.
“I think this place is about to blow up though, with f***ing COVID,” he says on a recording shared with Al Jazeera.
About a week later, a person infected with COVID was transported to a medical facility at Richard J Donovan, according to two inmates. During transit, the two prisoners said in recordings obtained by Al Jazeera, others were exposed.
“Richard J Donovan Correctional Facility (RJD) is following all proper protocols in its facility and during transit as outlined under CDCR/CCHCS Patient Movement Matrix and CCHCS guidance. Staff ensure all inmates that arrive at RJD maintain proper physical distancing, are quarantined for 14 days and are provided with proper testing immediately upon arrival back at the institution,” a CDCR spokesperson said in an email statement. “RJD responded to an increase in positive COVID-19 cases with robust coordinated efforts to increase the frequency of testing, conduct contact tracing and implement isolation and quarantine measures to mitigate spread of COVID-19.”
Johnson says her friend had tested positive on December 10. His phone time dropped to twice a week, and he used the time to call his family. Johnson did not hear from him for a month – a significant shift from the multiple calls per week they had before the pandemic.
While the cases have risen, family members of Richard J Donovan prisoners have been unable to reach their loved ones, and are left wondering if they are sick or in isolation.
“It’s the wildest response. In the regular world [a positive diagnosis] would be the moment that everyone starts calling,” says Bianca Tylek, the executive director of criminal justice advocacy organisation Worth Rises. “In the prison system, sometimes people’s families find out they have the virus because they haven’t heard [from] them.”
‘A big stress on families’
Even those who regularly receive phone calls and messages experience frequent problems.
Cammie Maturin, who co-founded a Louisiana organisation advocating for prison reform, regularly speaks with others whose family members are imprisoned. When she has tried to video chat with her fiance, an inmate at the Louisiana State Penitentiary in Angola, she has battled constant technical issues.
“It has been a big stress on families, not only emotionally, but financially,” she explains. “We’ve gone [from] talking two or three times a day to talking maybe once a week.”
The $1.4bn prison and jail telecommunications industry is largely controlled by just three companies. In 2019, a 15-minute call in Arkansas could cost $4.80, and $3.15 in Louisiana. Each message sent through JPay, one of the dominant electronics communications systems, costs anywhere between $.05 and $1.25, according to advocacy group Worth Rises. The costs add up quickly, with many facilities benefitting from monetary kickbacks built into the contracts.
“When the pandemic interrupted in-person visitation, Aventiv immediately began offering free communications and is proud to have provided 37.5 million free calls totaling 302.9 million minutes of free connection, 6.2 million free video connections, and 22.2 million free JPay Stamps for electronic messaging at hundreds of sites nationwide,” Jade Trombetta, a spokesperson for Aventiv, the parent company of JPay, wrote in a statement to Al Jazeera. “We will continue to work with our partners to continue to maintain connections between incarcerated Americans and their loved ones throughout the pandemic.”

Lockdowns have also increased the amount of items that prisoners need. With in-person education courses, vocational instruction and arts classes cancelled, family members send any entertainment they can afford.
Azzurra Crispino, the executive director of the advocacy group Prison Abolition Prisoner Support (PAPS), said she pays $28 and a $3 fee each month to provide her husband with streaming music. In the second half of December, she paid nearly $325 on phone minutes for her husband, who is imprisoned in Ohio’s Marion Correctional Institution.
“Getting the monthly music, which was something that before we maybe did as a treat, now has become a necessity. Sending him books, which before we did as a treat, now has become a necessity. Sending him more reading materials on JPay, also a necessity. Because he’s going more than a little nuts,” says Crispino, who last saw her husband on Valentine’s Day in 2020.
For “most of the pandemic”, she says, the prison provided fewer meals to her husband and other prisoners. She compensated by sending her husband food packages, purchased through a private company.
The Ohio Department of Rehabilitation and Correction (ODRC) said in an email statement that it did decrease the number of meals but raised the number of daily calories provided to prisoners from 2,500 to 2,725 calories.
“I am in a much better situation than most, and my car is held together by duct tape. If just calls were free, I could afford repairs or even a new car,” Crispino says. “We’re hearing from people who are saying I’m not paying on my electric bill to make sure that my child can talk to his father.”
Family members who spoke for this article said no amount of connection, at any cost, can ease the emotional strain of watching coronavirus tear through prisons. They worry about the masks their loved ones have used for months on end and the shared phones that are not adequately washed. They do not know when the next call will come. When they hear their loved ones are suffering, they wish they could help.
“He has been so down, and it scares me because he’s afraid he will die in prison, alone without his family,” says Patricia of her husband Rashiyd, who she married just five months before San Quentin shut down.
“This has been an agonising experience and some days it’s hard to even get up and work,” she adds. Even as she tries to buoy her husband’s spirits, she says, “this separation has caused me to sink into a deep depression, I’ve lost 40 pounds during this time due to stress. I have been to the [emergency room] multiple times, and after all types of testing I was advised that my symptoms were stress related.”

Vaccinations
As Christmas, the New Year and Valentine’s Day passed without visitations for the incarcerated, the COVID-19 vaccine has provided a glimmer of hope, though even that shred of optimism is tinged with distrust.
Margaret Breslau, the co-founder of the Virginia Prison Justice Network, says she hears from prisoners who do not want to take the vaccine.
“Many inmates either think that if they had COVID, they don’t need a vaccine, some think they should wait because they are afraid of secondary strains that would render this vaccine insufficient,” Breslau wrote in an email.
“The Department has a vaccine education campaign going and we’re trying to get as much information to both staff and inmates as we can,” Lisa Kinney, the Director of Communications for the Virginia Department of Corrections said in an email statement.
But in many states, those eager for the vaccine will have to wait. Although federal prisons across the country are distributing vaccines, some of the nation’s most populous state facilities, like those in Texas and Florida, are not inoculating inmates. After a lawsuit earlier in February, the New York corrections department said it was “preparing to vaccinate” prisoners aged 65 and older.
While the pandemic will likely leave a lasting scar on those outside prison walls, experts worry the damage will be deeper on those inside them.
“Our mind tends to hold on to the trauma in a way that even when we’re no longer in that setting of danger, our mind likes to sort of trick us into thinking we are. So even in safer settings, we still have those symptoms of PTSD and hypervigilance and being startled,” explains Kirandeep Kaur, a psychiatrist who has been evaluating undocumented immigrants held in ICE detention. “Those don’t go away unless there’s some sort of professional help.”